



|
|
|
Platelet-Rich-Plasma (PRP) & Micronized Fat (MFAT - Lipogems) UPDATE - Oct 2022
It has been a while since I updated the current status on use of Biologics in Orthopedics. Platelet rich plasma (PRP) and mesenchymal signaling cells (MSC) are the main biologics I will discuss. Amnion is no longer permitted in the US unless part of a clinical trial. We have been using PRP for over 10 yrs. and MFAT for over 6 years. Our experience has been very positive, and I continue to be an advocate of the use of these biologics in well informed patients who have not responded to traditional methods, such as anti-inflammatories, physical therapy or cortisone injection and as an alternative to surgery. It is important to note that PRP and MFAT will not heal a joint that is having mechanical symptoms such as giving way, locking or instability. I just attended 2 meetings on the use of Biologics in Orthopedics called the Biologic Alliance. Many of the world's best thought leaders and clinicians shared their experiences and opinions on the current indications and use of these biologics. This blog will focus on recent recommendations from the conferences about platelet rich plasma (PRP) and MFAT (Lipogems), how it works, and where it works, and where it does not. The use of PRP (platelet rich plasma) is a very straightforward procedure that involves taking blood in the office, spinning it down, concentrating the platelets and injecting it into arthritic joints. It's best to use PRP that is low in white cells so there is less inflammation for joints. (yellow PRP, not red). The "red" PRP may be better for injecting tendons as having inflammation in a tendon will signal healing. There have been several excellent studies that have shown that PRP is superior and lasts longer than cortisone or hyaluronic acid or lubricant injections. See articles below. PRP or MFAT have been shown to be helpful in not only the knee, but other joints as well, although there is not as much data in the shoulder. It does NOT heal a completely torn rotator cuff but may be helpful in partial tears. Injections can be repeated, unlike cortisone, which has its long-term negative effects and is best used in acute inflammation. For example, cortisone works very well when you can't walk because the knee is acutely swollen and painful, or a calcium deposit in the shoulder. In Europe, where most of the long term studies have been done, an initial 2 injections and yearly thereafter has shown the strongest results. Results are not as predictable in severe bone on bone arthritis. PRP was initially used for tennis elbow and continues to show excellent results in chronic tennis elbow, Achilles tendinosis, hip "bursitis" and a bit less predictable results in patellar tendinosis. This is an option when all non-interventive treatment fails. It is important to remember that PRP is NOT the first treatment that should be used. It has also shown benefit in acute muscle tears or ligament sprains. The use of PRP for tendinitis of the rotator cuff and for surgical treatment of rotator cuff tears has not been shown to be superior to placebo in a large Level One study, and there are no studies that show that injecting PRP for partial rotator cuff tears or chronic impingement is any better than steroids or Toradol. The use of a membrane of PRP HAS been shown to improve the healing and reduce the re-tear rate in large to massive cuff tears. We first started using this membrane in 2004 and have had a similar experience. What's better? 1 injection ...3 injections? There are decent studies on both sides. One study comparing 2 vs 1 injections, showed no difference. (Patel). However, a new double blind randomized study (Gomelli) showed for mild to moderate osteoarthritis of the knee, 3 injections had significantly better results at 6 months than a single PRP injection or HA (Orthovisc), although all improved over a control with saline injected. For advanced OA, 1 injection showed improvement and there was no advantage to 3 injections. My approach has been to do two injections, and repeat as is necessary, or if the pain begins again. This new study will change my protocol. We are respectful that these are not covered by insurance. Injections for the Treatment of Arthritis- PRP, Lubricants (HA) and Micronized fat There have been some important papers published in the past year comparing the benefits of injection of platelet rich plasma (PRP), hyaluronic acid (HA) and saline (placebo). These papers show statistically significant improvement in pain relief with platelet rich plasma over HA and saline. These findings offer an additional weapon in treating pain in patients with moderate osteoarthritis. Steroids last about 1-2 months, HA can last up to 3 months and PRP up to 9-12 months. As an introduction, for decades steroids (cortisone) has been used to treat the swelling and pain of osteoarthritis. Arthritis can be mild (Grade 1-2), with softening of the cartilage that covers the end of the bone, to moderate (Grade 2-3), to severe, when the cartilage is worn down to bone (Grade 4). It has been very successful in relieving swelling and offers short term improvement in pain, but long-term relief is not as predictable. It is low cost, easy to administer during an office visit, and does not require lengthy authorization and paperwork from the insurance companies. However, repetitive use of steroid injections is not healthy for the articular cartilage in any joint or tendon and can increase the risk of infection should surgery become necessary. It is usually restricted to at most 2-3 a year in most cases. (This is different if the patient has rheumatoid arthritis or inflammatory arthritis, which is a different problem); Many insurance companies now require a trial of a cortisone injection before use of HA. HA has also been increasingly NOT covered by insurance companies as well and does not last as long as PRP. PRP is not covered by insurance companies, except some Workers Compensation companies. . Because of the limitations of cortisone or steroid injections, hyaluronic acid injections were developed to try to replace some of the chemical imbalance seen in the knee in osteoarthritis. The claims that HA can regrow cartilage in some of the advertising media is just not true. It acts to relieve pain in 70% of patients for up to 3-6 months in many of the series published. It is quite expensive and requires authorization from the insurers. The patient receives one to 5 injections a week apart, but most companies have 3 injections. (There are several companies that sell HA such as Synvisc, Eufflexa, Orthovisc, or Suppartz). The risks are small, from swelling after the injection, allergic reaction to the medication, and infection. Many insurance companies are not covering this anymore. Platelet rich plasma has been used in many areas of musculoskeletal care. PRP is prepared from the patients' own blood, and involves taking a small amount of blood, and separating the platelets from the red cells and concentrating the platelets so they can be injected into the knee. This is done in the office and the injection is done at the same visit. Comparative studies have constantly shown its superiority over steroids and HA alone. Some recent studies show that PRP + HA together can provide additional benefit. Bone marrow concentrate and Micronized fat have more growth factors than PRP and a few stem cells- fat 100 times more than bone marrow, but the benefit comes from the "bioactive" cells and enzymes that turn off the inflammatory cells and turn on the ones that can stimulate healing and pain reduction. There are studies on both sides and our own experience has shown 75% of patients found the Lipogems or micronized fat to have been helpful in 2-4 year followup. There is more information in the brochure under orthobiologics. We recommend the Lipogems for patients that have had part of their meniscus removed as part of our approach to avoiding progression of their arthritis, mild-moderate arthritis, or in cases of patients wanting to try alternatives to total joint replacement. 3 good peer reviewed articles
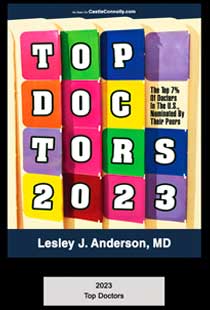
Current Focus: As one of America's Top Doctors for 22 years and a very busy surgical career, Dr. Anderson's current focus is to help patients with osteoarthritis, rotator cuff injuries and other shoulder and knee injuries get the most complete education and treatment on what works and what doesn't work as they wade through all the social media advertising that one can be overwhelmed with. Each patient is different, and education is key to making an informed choice about their own body. We hope to provide that for you and get back to the doctor -patient relationship without the time constraints of insurance. Some of the questions we take the time to deal with treat are: Do biologics work? What are biologics? Is PRP right for me? What can I expect with a total knee replacement? When is the right time? What is all this about "stem cells" and regenerative medicine? Does it work? I am not ready for a total knee, what other treatments are available? What surgical and nonsurgical options are available for my specific condition? I am also still committed to treating Work injuries for the City and County of SF and San Mateo firefighters and police officers. They need the best care possible for all the brave and heroic service they provide to us. PRACTICE CHANGES as of 7/1/22 To my wonderful patients; I wanted to let you know that as of June 1, 2022, I terminated my contracts from all PPO, Brown and Toland, Medicare and HMO plans. I am not retiring and still operating and seeing patients, but after 35 years in practice, I wish to make life a bit simpler and still offer the kind of care most of you have become accustomed to from me and my wonderful staff. I have moved to a new office across the hall in Suite 332. I hope you will choose to continue care with me as many of you may have coverage out of network. Your health plan would still cover MRIs, Surgery centers costs, PT, just not my fee. We can also assist in submitting your bill to your health plan if you want us to. Your employers benefit manager may also be able to help you with that as well as to the specifics. If you choose to seek care from an in-network physician, we will provide your records to you or your new provider, if you send us a written request. I love caring for and about patients, and I regret the intrusion into our relationship. I have been honored to have your trust to serve as your physician and hope I can continue in that role in the future. If you need a name of a new surgeon, call us and we can give you some recommendations. With warmest regards. Dr. Anderson Mission Statement: Our mission statement has not changed after 38 years in practice. But our focus has. We continue to individualize each patient's care with the focus on finding the best solution, be it nonsurgical or surgical for each person's orthopedic problem. We develop long-term relationships with our patients and strive to provide a comfortable environment for patients to receive help with their orthopedic problems. The Anderson Knee and Shoulder Center, located at 2100 Webster Street, Suite 332 in San Francisco, is the office of America's and San Francisco's Top Orthopedic Surgeon Dr. Lesley Anderson. She helps patients choose the best nonsurgical or surgical options for knee, and shoulder. Re: Covid 19 We hope you have been vaccinated and/or will be soon. Based on current mandated guidelines, we cannot see anyone at the office who has any of the following:
Wishing everyone good health, and hope for a better 2022-23, and know that your safety and good health are in our thoughts and prayers. Patient Reviewspowered by BirdEye |
   |